DOREMY
What is the DOREMY trial?
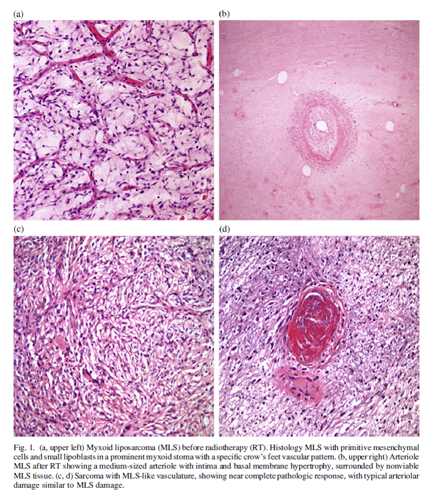
The international DOREMY trial (NCT02106312) was initiated in 2010 for patients with myxoid liposarcomas (MLS), soft tissue tumors in the arms or legs. This study investigated whether a reduced dose of radiotherapy before surgery could be equally effective against this condition while minimizing side effects.
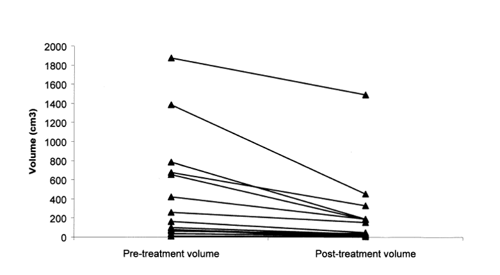
Patients received preoperative radiotherapy with a reduced dose of up to 18 x 2 Gy instead of the usual 25 x 2 Gy. One hundred patients participated in the trial, which was completed in August 2019.
What were the results of the DOREMY trial?
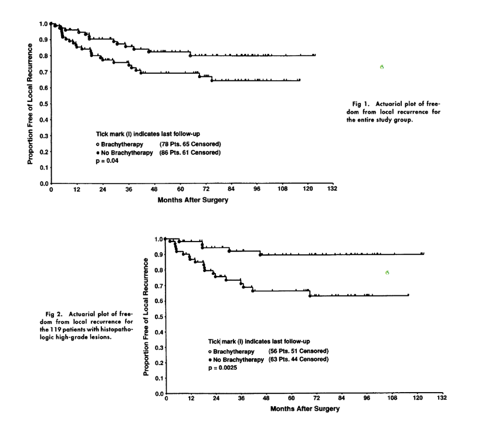
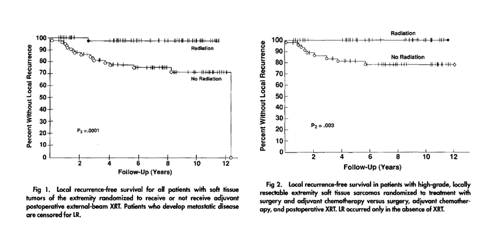
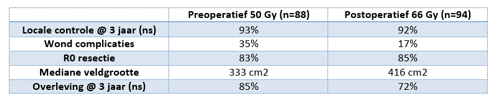
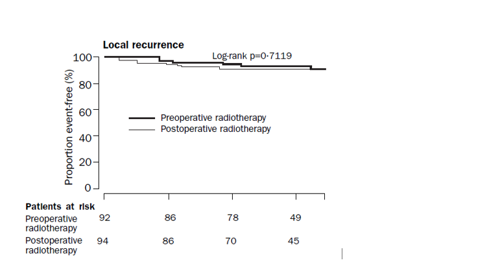
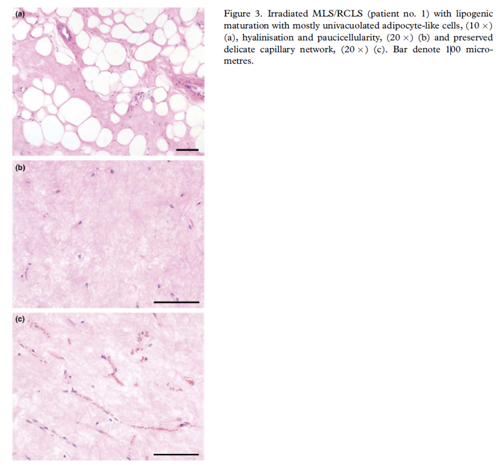
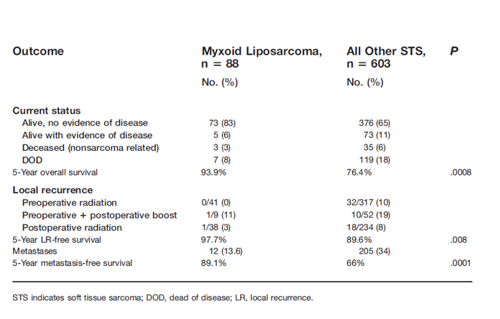
The median follow-up of the first 79 patients is now over two years. They have been treated for MLS with no metastases at the time of diagnosis. Local control at two years was 100%. When studied under the microscope, 91% of patients showed an extensive pathological treatment response to the reduced dose. Only 17% of patients experienced problems with wound healing after surgery, whereas a 35% chance would have been expected (historically) when opting for 25 x 2 Gy (see also O'Sullivan's SR-2 trial).
The full results of this trial were presented orally on November 12, 2020, during the annual Connective Tissue Oncology Society meeting (CTOS) and published in the leading journal JAMA Oncology. The results were presented by Jules Lansu, a PhD student working on this trial.
 nl
nl
 Nederlands
Nederlands