Surgery for cancer in the oral cavity and throat
Surgery to the oral cavity or throat can be very drastic. The specifics of the treatment depend on the stage and development of the disease.
If your tumor is small, it can be surgically removed together with the surrounding tissue — the margins — with a robot or laser beam. We will then close the wound with stitches.
If your tumor is larger, we will perform a COMMANDO procedure. This is an extensive operation, taking between 8 and 10 hours, involving a head and neck surgeon and a reconstructive surgeon. Together, they ensure that the final result will look as nicely as possible and that the patient retains as much of their function as possible.
More information
Surgery to the oral cavity or throat – what to expect?
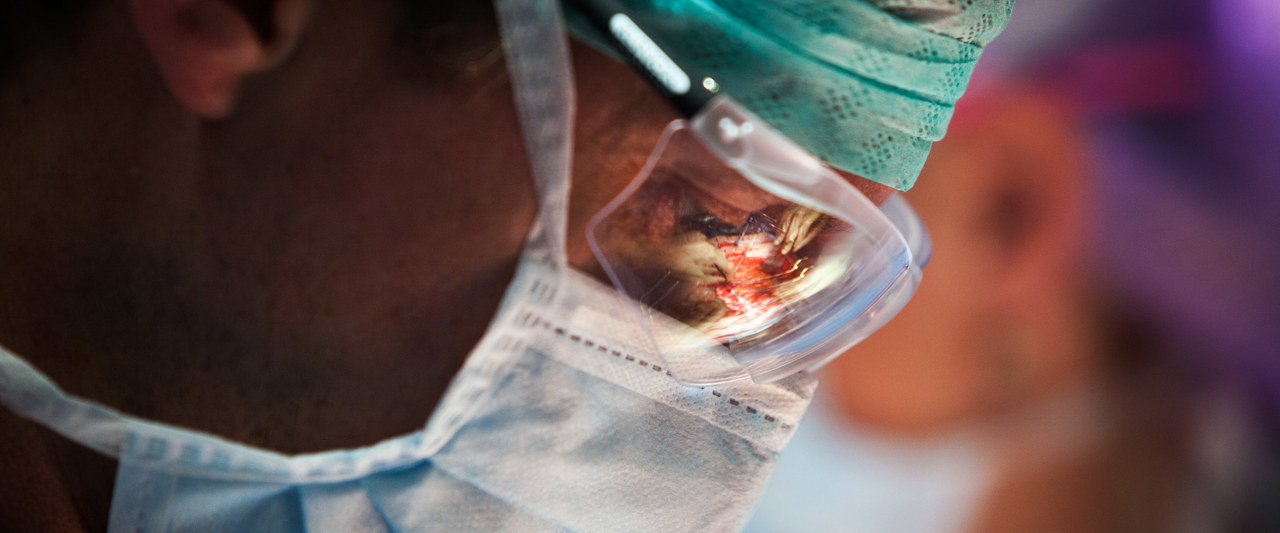
Tumors in the oral cavity or throat are removed under general anesthesia. The procedure will involve two specialists: a head and neck surgeon and a reconstructive surgeon.
No matter its size, the tumor will be removed together with its margins. This can be tissue from the tongue, the bottom of your mouth, the soft palate, or even a piece of your bottom jaw. If we have reason to believe that the lymph nodes in the neck may be affected, they will be removed. Your surgeon may want to preventatively remove these nodes even when the cancer has not spread. because tumors in the oral cavity or throat can spread to the lymph nodes in the neck at an early stage in their development.
If a significant amount of tissue needs to be removed, your surgeon will fill this gap using a transplant. This can be a piece of skin, muscle, or bone from another part of your body such as the chest, forearm, or lower leg. If part of your jaw has to be removed, your surgeon will use metal or bone from your lower leg to craft a prosthetis.
Effectiveness
Cancer in the oral cavity or throat can be treated effectively with surgery. The risk of recurrence, however, remains.
This is why we will invite you to come in for regular screenings for at least 5 years. These screenings will decrease in frequency after the first few months.
Preoperative screening
Before your surgery, you will be invited to meet with your anesthesiologist at the outpatient clinic for a consultation and a brief examination to assess your overall shape and any potential particularities we will need to keep in mind. The consultation assistant will measure your heart rate and blood pressure and will inquire about your height and weight. If needed, we can take those measurements during the appointment.
This preoperative screening will take approximately 20 minutes and will form the base of your anesthesia. Your anesthesiologist will listen to your lungs and heart and inspect your mouth and throat in preparation of the breathing tube that will be placed during surgery. Your anesthesiologist will also ask you:
Before your surgery, you will be invited to meet with your anesthesiologist at the outpatient clinic for a consultation and a brief examination to assess your overall shape and any potential particularities we will need to keep in mind. The consultation assistant will measure your heart rate and blood pressure and will inquire about your height and weight. If needed, we can take those measurements during the appointment.
This preoperative screening will take approximately 20 minutes and will form the base of your anesthesia. Your anesthesiologist will listen to your lungs and heart and inspect your mouth and throat in preparation of the breathing tube that will be placed during surgery. Your anesthesiologist will also ask you:
- whether you have been under anesthesia before
- whether you have any other conditions
- whether you have taken cancer medicine before
- whether you have had radiation treatment before
- whether you have any allergies
- whether you smoke
- whether you drink alcohol
- what kind of medication you take
Please inform your anesthesiologist of the type of medication and dose you take, and how often you take it. Your physician may want to run more tests before your surgery, such as: electrocardiogram (ECG), lung x-rays, a lung function test, or a blood test.
General or local anesthesia
Before your surgery you will be given general anesthesia, local anesthesia, or a combination of the two. General anesthesia means that you will be completely unconscious during surgery, whereas local anesthesia means that a part of your body will be numb and motionless.
General anesthesia
General anesthesia completely sedates your body. You will be given a cocktail of sleeping medicine, pain killers, and sometimes a muscle relaxant through IV. You will be unconscious within 30 seconds. You will be ventilated during the entire process.
If you are having major surgery, we will place a respiration tube in your throat. For smaller surgeries, a small cap in the back of the throat will suffice. We will closely monitor your heart rate, blood pressure, breathing, and temperature through our monitoring devices.
Local anesthesia
If you are given local anesthesia, you will be conscious during your surgery. Local anesthetics are usually administered through an epidural in the spine, and will temporarily numb all body parts underneath. We may place a tube to give you IV pain medication during and after surgery.
Your anesthesiologist will keep a close eye on your blood pressure, heart rate, breathing, and temperature in order to adapt the anesthesia if needed.
Most people undergoing major surgery will be given a mixture of general and local anesthetics.
Side-effects and complications
You may feel discomfort in the neck or shoulders as a result of the removal of the lymph nodes. Lymph fluids may build in your face. Lymphatic drainage therapy may alleviate your symptoms.
You may also experience trouble breathing due to a temporary swelling as a result of the surgery. Your physicians can create a hole in your trachea to help you breathe. This hole will be kept open by a small pipe (canule). Once you are able to breathe by yourself, we will remove this pipe so the hole can heal. Only in rare cases will this pipe need to remain in place. If tube feeding is required, this will most likely be temporary as well.
Your mouth and throat function may be affected, depending on the complexity of your surgery and radiation treatment. You may experience trouble articulating, swallowing, or chewing. The severity of these symptoms depends on the complexity of the surgery and (preventative) rehabilitation.
After your surgery
The margins will be tested for cancer cells. If we find cancer cells in the tissue or lymph node, you will require further treatment with radiation therapy or chemotherapy.
Because you will be temporarily unable to eat due to your surgical scar, we will place a tube for feedings. Your practicing physician and dietician will help you reintroduce solid food once you are ready.
 nl
nl