Surgery for lung cancer
A team of specialists at the Netherlands Cancer Institute will support you through your surgery. This team consists of medical specialists, [physician assistants and clinical nurse specialists. Our (thoracic) surgeons closely collaborate with our pulmonologists (lung specialists) during your surgery, while our anesthesiologists handle your anesthesia and pain treatment. Our physical therapist can help you prepare for the surgery and support your recovery.
Knowing you have to have thoracic surgery can be stressful and uncertain. To support you and your lived ones through this period, our clinical nurse specialists will be your direct contact point during the entire process.
Meet our NKI Lung Cancer Center team, or read more about the different types of thoracic surgeries available at the Netherlands Cancer Institute as well as our care.
We have combined all our information about the lungs and thorax on this page, as the two are anatomically related.
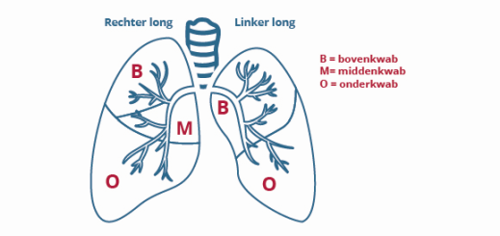
The lungs - position, structure, and function
The right and left lung are found in the chest (thorax) on both sides of the heart. The right lung has three lung lobes, while the left lung has two. Every lung is covered by a membrane, the pleura. The area between the lungs is called the mediastinum. This is where you will find the heart, trachea (part of the airways), esophagus, blood vessels, nerves, lymph nodes and lymphatic vessels.
The air you breathe in through your nose or mouth reaches the lungs through your oral cavity. The airways lead to two large branches that lead to the lungs, where they branch out even further into the small vesicles. The lungs take in oxygen.
When is surgery an option for you?
Whether surgery is an option for you, and whether it will be beneficial, depends on the location and size of your tumor and whether it has spread to the lymph nodes or other places in the body (the other lung, or other organs). We may not be able to remove your tumor without (too much) harm - like if your tumor attached itself to your heart. We may be able to remove your tumor but not the metastases. This means it is not very useful to remove it.
Your personal situation may be different from the examples above.
The NKI is a training hospital. Your treatment team may include PhD students training to become surgeons as well as surgeons working towards specializing in pulmonological surgery.
Lung or thoracic surgery may be needed for one of the following reasons:
- We usually use surgery to treat lung cancer or lung metastases from malignant tumors elsewhere in the body
- A rare disease of the pleura caused by asbestos (mesothelioma)
- Soft tissue tumors that occur in the lungs, ribs, or muscles of the chest wall (sarcomas)
- Rate tumors behind the sternum (mediastinum) like thymoma
- Infections, benign abnormalities, or unknown abnormalities.
Types of thoracic surgery
If surgery is an option for you, your surgeon will opt for the safest method that will cause the least pain or complications. We will discuss the treatment plan with you during a consultation at the clinic. Surgeries can be divided by the type of procedure, and the technique used. The type of procedure will depend on the part of the lung that will need to be removed. The technique concerns the method or approach used during surgery. Whenever possible, we will opt for laparoscopic surgery (thoracoscopy or VATS) or robot assisted surgery (RATS). Some people will need to undergo a classic approach (thoracotomy or sternotomy). More than 70% of surgeries in the Netherlands are laparoscopic or robot assisted.
Types of procedures
Below are images of two types of procedures. We expand more on them on this page.
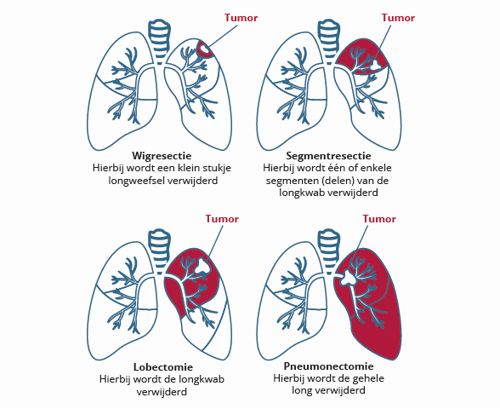
What is a pneumonectomy?
A pneumonectomy is a surgical procedure to remove a lung - either the right side, or the left. This is a major surgery that can only be done if the other lung functions well. This procedure is usually done through the classic approach (thoracotomy).
What is a lobectomy?
The left lung has two loves, and the right lung has three. A lobectomy is a surgical removal of the lung lobe which has a tumor. The lymph nodes next to the tumor will be removed as well. We can use an open surgery technique (thoracotomy) or laparoscopic surgery (VATS) or robot-assisted surgery (RATS).
What is a segment resection?
The lung lobes consist of various segments. A segment resection is a surgical procedure to remove one or more of these segments. This procedure can remove certain tumor types in the lung. This type of surgery will usually be laparoscopic (VATS).
What is a wedge resection?
A wedge resection is a surgical procedure that remives a part of the lung lobe in the shape of a wedge (a pizza slice). This surgery aims to remove metastases in the lungs. The tissue will be send to a pathologist for analysis. This surgery can be open surgery (thoracotomy), but is usually laparoscopic (VATS).
Surgery for mesothelioma, asbestos cancer
Under very specific circumstances patients with mesothelioma can have surgery. Surgery for mesothelioma is not always beneficial. Surgery is only done as part of a trial, for a small number of patients.
Surgery for tumors behind the sternum (mediastinum) like thymoma
if you have an abnormality behind the sternum, like a thymoma (a tumor of the thymus), you may need surgery to remove it. We can remove it with a RATS or sternotomy procedure. Depending on the exact abnormality and its location, your surgeon will decide which option is best for you.
Surgery techniques
What is a VATS?
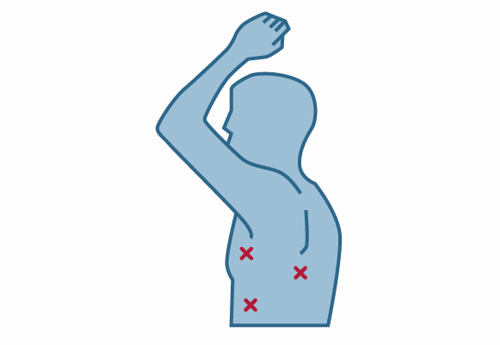
VATS stands for Video Assisted Thoracic (or Thoracoscopic) Surgery. It is a surgery of the thorax (chest) using a surgical camera and video monitor. The VATS is a keyhole, or laparoscopic surgery, also known as a thoracoscopic procedure.
We use a thoracoscope for laparoscopic surgeries: a time with a small camera and light attached to the end. The thoracoscope is connected to a TV monitor allowing the surgeon to see the surgery.
Your surgeon will make 2 to 4 small incisions in the skin between the ribs. See the image below for the exact placement. To allow for sufficient space, the anesthesiologist will collapse the lung requiring surgery by halting your breathing to that lung while you will receive your oxygen through the other lung. Your surgeon will insert 2 or 3 tubes into the thorax through the incisions. The surgeon can see the inside of your body on the screen connected to the camera, so a large incision won’t be necessary. Your surgeon can then remove the tissue using instruments inserted through the other tubes. Smaller tumors or entire lung tubes can be removed using special staplers. After the procedure, the incisions will be stitched back together and your lung will receive oxygen again, reinflating them to their usual shape.
Not all tumors can be removed through VATS. If your tumor attached itself to the lung tissue, or if you have received radiation therapy in the past, or if we cannot properly see the abnormality or if we encounter unforeseen complications of bleeding during surgery. During the surgery, we may find out that your situation is more complex than we had initially thought. Your surgeon may need to make a bigger incision (thoracotomy) to properly treat you.
What is a RATS?
RATS stands for Robot Assisted Thoracic (of Thoracoscopic) Surgery. We use a RATS to remove tumors in the lungs and behind the sternum. A RATS is a laparoscopic (keyhole) surgery, just like a VATS. The only difference is that all operations are done by a robot controlled by your thoracic surgeon, who is seated in a ”cockpit”. The robot gives the surgeon an enlarged and 3D image of the area which allows for great precision. Because the robot is beneficial in certain kinds of surgeries compared to the VATS, the robot is only used if this procedure has an advantage. Recovery time after RATS is usually quicker than after open surgery (thoracotomy or sternotomy).
What is a thoracotomy?
A thoracotomy is a surgical procedure which opens the chest to access the chest cavity or lungs. Your surgeon will make an incision between the ribs (on the left or right side). The exact location will depend on the location of your abnormality.
What is a sternotomy?
A sternotomy is a surgical procedure in which your sternum is opened vertically. After making an incision in the skin, your surgeon will saw through the bone of the sternum. This allows your surgeon access to the chest to remove the abnormality. The sternum will be sewn back together using steel wire, allowing it to close. These wires won’t need to be removed and can remain in place indefinitely.
Before surgery
Diagnostic tests
To prepare for your surgery, we will need to do several diagnostic tests (scans, long function). Your surgeon or pulmonologist can tell you more about this.
The following diagnostic tests may need to be run before your surgery:
- An ultrasound of the esophagus (EUS) or windpipe (EBUS). We can take tissue biopsies during the procedure.
- CT guided biopsy: using CT scan imaging we can take material for analysis.
- Mediastinoscopy: the lymph nodes behind the sternum and windpipe are examined, and tissue is removed for analysis.
Staff
You will see the following people at the clinic:
- The thoracic surgeon is responsible for your surgical treatment. You can contact him or her if you have questions about the procedure.
- The pulmonologist is involved in treatment of nearly all patients with lung problems. Before and after your surgery your polmonologist is involved in your medical treatment and he or she will arrange follow-up care. Your pulmonologist will also give you chemotherapy or radiation therapy if required.
- The anesthesiologist manages your anesthesia and pain treatment. He or she will ask you about which medicines you take and will let you know which ones you can take before your surgery. If you need to stay at the Intensive Care unit after your surgery for observation, your anesthesiology will be your practicing physician during your stay.
- Clinical nurse specialists thoracic surgery: your primary contact person in the time surrounding your surgery.
- Your consultation with a nurse at the clinic can prepare you for your admission. The nurse will carry out a medical questionnaire, and there will be plenty of time to ask questions, or request additional information.
- The physical therapist can give you instructions on coughing and practice breathing techniques with you. This will help prevent complications like pheumonia after your surgery.
What can you do before your surgery?
For a proper recovery after surgery, it is important to be in the best health possible. Consider giving up smoking and alcohol, or eat healthy and exercise.
After surgery you will have a surgical wound (on the inside and outside of your body). Research has shown that wound healing is faster if you do not smoke. The risk of pneumonia increases in smokers. It is very important to quit smoking before your surgery to allow yourself the best recovery possible.
The addictive substance nicotine may make it hard to give up smoking. Please consider quitting before your surgery. The nurses at the smoking cessation clinic can offer support. Your physician or nurse can give you more information.
Smoking cessation clinic
Our staff at the Smoking cessation clinic can assist you when you quit smoking. They offer a specialized treatment program that emphasizes changing your habits.
During and after surgery
The day of the procedure
Depending on the procedure you are having, you will be admitted to the hospital one day before, or on the day of the procedure.
Your nurse will take you to the prep room to prepare for surgery. One of the OR employees will welcome you there. Your surgeon and anesthesiologist will also be nearby. Your surgical team will run through a checklist and may ask you some questions.
You will receive an IV before your surgery so we can give you the anesthetics. We usually insert a small tube into your back, an epidural catheter, to administer painkillers during surgery.
The days following the procedure
You may have to spend a night at the Intensive Care after the procedure. Your anesthesiologist will oversee your medical treatment and check-ups. He or she will determine when you can go back to the regular ward together with your surgeon. Most patients will have to spend several hours in the recovery room before being brought back to the ward.
The department physician will see you every day to discuss your recovery together with your nurses. You can discuss new agreements during these visits. The department physician will discuss your progress with your practicing physician. Your surgeon will also see you regularly.
Recovering lung functionality is our top priority. Your nurses (and physical therapist, if needed) will give you advice and exercises to improve your breathing and to help you cough up mucus from the airways.
The results
if tissue has been removed during your procedure for analysis, you will receive the results after 5 to 7 weekdays. Your pulmonologist or thoracic surgeon will discuss these results with you at the in or outpatient clinic, depending on where you are in your recovery. This consultation will involve your results, any potential follow-up care, and your prospects.
Treatment as part of a trial
The Netherlands Cancer Institute conducts research into the treatment of lung cancer, pleural cancer, tumors behind the sternum, and metastases. Depending on your personal situation, you may be asked to participate in a trial.
Regular treatment may not be effective enough for you. If you qualify for a more expermental treament, your physician will provide more information.
Leaving the hospital
When you can leave the hospital will depend on the surgery you have had, and the speed of your recovery. We always aim to let you go home as soon as possible, after an average time of 3 to 7 days, depending on your surgery.
You may need more care after leaving the hospital. Please discuss this with your physician and nurses.
Your nurse will have a discharge consultation with you and a loved one, if you wish them to be present. During this consultation we will reflect on your time at the hospital, and prepare you for the time that lies ahead after your hospital stay. We will also plan an appointment for follow-up screenings at the clinic.
De periode na het ontslag
Na het ontslag uit het ziekenhuis kunt u uw dagelijkse activiteiten weer geleidelijk uitbreiden tot uw normale niveau. Zorg daarbij voor een dagritme waarbij na activiteiten rustmomenten ingelast zijn. Het is moeilijk aan te geven wanneer u weer helemaal van de ingreep bent hersteld. Dit hangt af van de grootte en de complexiteit van de ingreep, uw conditie en eventuele voor- of nabehandeling.
 nl
nl